“What can we do at this critical moment in time, with a vulnerable population, with a workforce shortage and without more resources? Connect-Home empowers staff in affordable housing, focusing on getting the right people where they are needed and creating a community of care.”
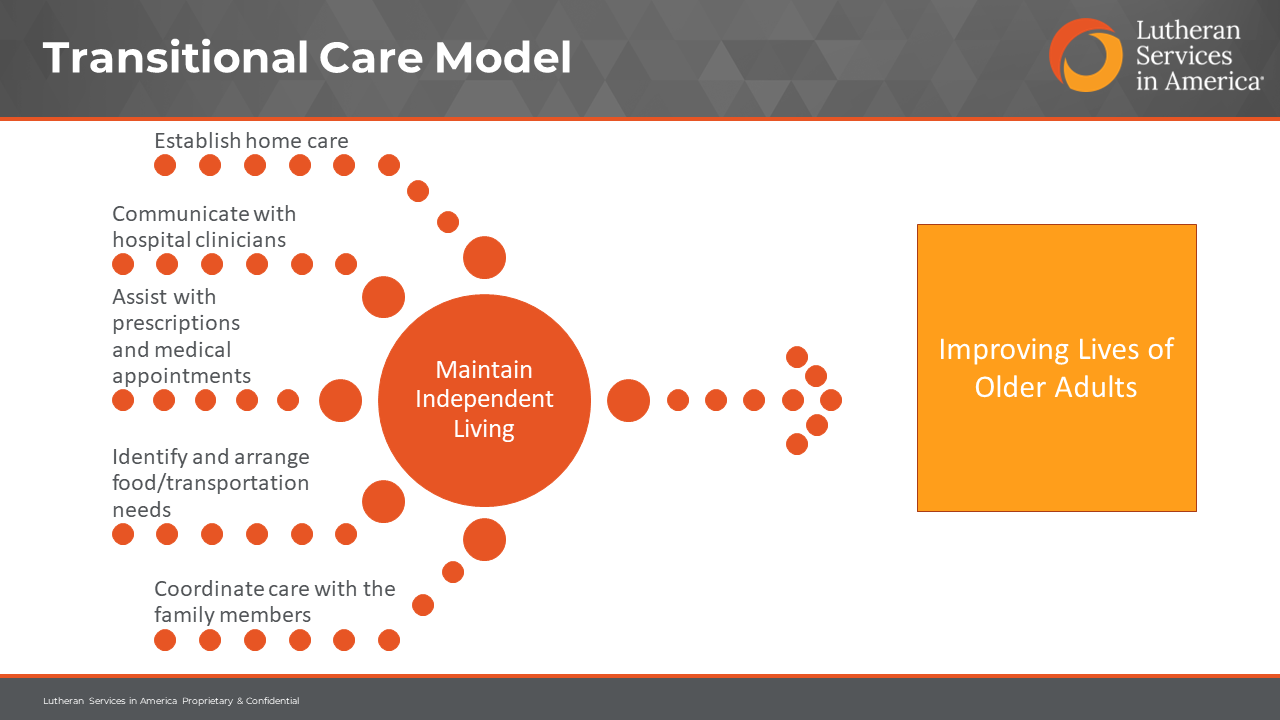
This was the lead message of a joint presentation to Grantmakers for Housing Stability in Aging on April 12 by Susan Newton, Senior Director of Strategic Initiatives at Lutheran Services in America, about the innovative Connect-Home model. The model, which is being implemented with Lutheran Services in America support in two senior affordable housing units in Brooklyn, New York, aims to improve the health and social outcomes of older adults transitioning home from an acute care experience, including prevention of rehospitalization.
As Newton, Kathy Hopkins of our member Family Health Centers at NYU Langone, and Mark Toles of the University of North Carolina-Chapel Hill described, the model is uniquely working to partner with on-site resident service coordinators (RSCs) to build a caring community of support to the diverse and medically high-need populations—36 percent of whom are over age 86 and 45 percent of whom list a Chinese dialect as a native language—in the affordable housing units targeted.
Toles, who pioneered the use of Connect-Home for patients transitioning out of skilled nursing facilities, noted how adaptation to affordable housing has been an exciting and sometimes surprising collaborative process with RSCs, senior residents and Family Health Centers at NYU Langone.
“The staff really had minimal awareness of hospital stays. They had an intuitive sense that a recent hospital stay was something to be concerned about but did not have procedures to routinely identify and support [senior residents],” said Toles.
He noted that bringing rigor to the identification of residents with a recent acute care stay was one of the biggest hurdles for getting Connect-Home off the ground. A surprising asset was a log maintained at the front desk tracking ambulance visits to the facility. That list has become a key tool to identify vulnerable residents and engage in follow-up.
The essential transformation was with RSCs, who have started to embrace the model as a key, not ancillary, part of their role. As Hopkins noted, “They came from ‘I cannot add one more thing to my plate’ to ‘This is such a good way of working and prevents older adults in our community from going back to the hospital.’”
Toles noted some of the seemingly small tasks that RSCs help returning residents with that make a difference, such as tracking down lost discharge instructions or ensuring supportive home care is provided on schedule. RSCs are also being trained to connect residents with more complex follow-on needs to additional community support.
All partners noted how Connect-Home continues to evolve, with care teams meeting regularly to improve the process, analyze data and improve gaps in identification and services.
To learn more about this Lutheran Services in America-led learning collaborative, please reach out to Susan Newton.
Kent Mitchell is Vice President of Strategy & Innovation at Lutheran Services in America.